Eight out of ten people suffer from back pain at some time during their lives. Back pain is the second most common reason people visit healthcare provider. In people under 40 years of age, back pain is the most common reason for the inability to perform daily tasks.
Pain that primarily affects the back should be distinguished from a spinal condition that results in mostly sharp shooting leg pain, a condition commonly called sciatica. Typically, sciatica is the result of a “pressed nerve” in the lower back. In most cases, the cause of the sciatica is clearly defined; for example, a disc problem or arthritis. The cause of an episode of back pain, on the other hand, often is more difficult to pinpoint, and may be related to the discs, joints, or soft tissue supports (muscles, ligaments and tendons).
What is acute back pain?
Acute back pain refers to a brief episode of pain that comes on suddenly. Most people recover from acute back pain within two weeks with minimal treatment. Using commonly available pain relievers – such as paracetamol or ibuprofen – and getting back to normal activities as the pain permits are simple and effective treatments for most people with acute back pain. Hot fomentation and applying pain relieving gels or oil can also help.
What is chronic, persistent back pain?
Most back pain is relieved within a few days to a couple of weeks with simple treatment. When back pain persists beyond four weeks, further medical evaluation is required. This evaluation focuses on a careful assessment of the patient’s medical history and a thorough physical examination to identify, if possible, a precise cause of the pain. More commonly, the pain is related to weak back muscles, the spinal joints, or prolapsed discs.
What causes back pain?
Back strain due to weak muscles
Back strain along with weak back muscles is the leading cause (85 percent of cases) of back pain. Bad sitting postures, prolonged travel or work, bad mattresses, etc add to back strain. If back muscles are not exercised regularly, back pain arises.
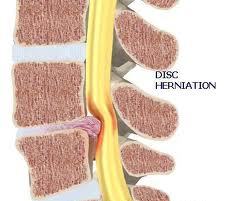
Disc herniation (2 percent of cases) – A herniated disc is a rupture or tear of the cartilage that surrounds the vertebral discs. Pressure from the vertebrae above and below the affected disc squeezes the cushioning substance (nucleus pulposus) out of the disc. The nucleus pulposus can press against spinal nerve roots. This can cause severe leg pain and may cause nerve damage if not treated properly.
Osteoarthritis/spinal stenosis (1 percent to 2 percent of cases) -This is characterized by the constriction or narrowing of the vertebral canal, the space that surrounds the spinal column.
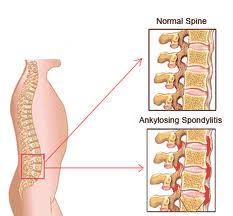
Ankylosing spondylitis (less than 1 percent of cases) – Ankylosing spondylitis is a chronic inflammatory disease that first affects the spine and adjacent structures. As the disease progresses, vertebrae will fuse together. This disease has a strong hereditary tendency and primarily affects men under 30 years of age.
Spondylolisthesis (3 percent of cases) – Spondylolisthesis is the partial forward movement (dislocation) of one vertebra over the one below it. Usually, the fifth lumbar vertebra is dislocated over the first sacral vertebra.
Infection and Cancer are uncommon causes of back pain.
Fracture (4 percent of cases)
Trauma – An injury due to an accident or fall may cause a fracture or muscle strain.
How is back pain diagnosed?
Evaluating the patient’s medical history often is the doctor’s most powerful diagnostic tool. The doctor asks a series of questions to help identify possible causes of the back pain. The questions may focus on lifestyle factors, such as where you live, what type of work you do, and what activities or hobbies you enjoy; when your pain began; where your pain is located and what effect it has had on your daily activities; and whether your pain has responded to any treatment. The doctor also will ask about your medical, surgical, family, and social history.
Extensive testing – including X-rays, MRI/CT scans, EMGs, and lab tests – are necessary in some cases. These tests may demonstrate common degenerative, or “wear and tear,” changes in the discs or joints in the spine. If the pain is caused by trauma or a neurological change, or if the patient has a persistent fever, is losing weight, has numbness or weakness or loss of bowel or bladder control, one or more of these diagnostic tests may be done immediately.
How is back pain treated?
Most back pain can be successfully treated with conservative (non-surgical) measures. Conservative treatment includes activity (standing, walking, working) as tolerated, acetaminophen (non-aspirin over-the-counter pain reliever), and/or an anti-inflammatory medication, and cold packs to diminish swelling and pain. Usually, the pain will subside within four to seven days. If there is no improvement after four to seven days, contact your doctor.
When back pain is chronic, persistent and disabling, a comprehensive treatment approach addressing all aspects of the problem, including psychological as well as physical, offers the best hope for rehabilitation and recovery. A multi-disciplinary treatment team – consisting of a Neurologist, orthopedician and physiotherapist – offers the best hope for return to an active, productive lifestyle.
Medication
The role of medication in the management of back pain is to relieve symptoms and facilitate an active, exercise-oriented rehabilitation program.
Exercise
Active, exercise-oriented physical therapy is the cornerstone of treatment for people with chronic back pain. Heat, ice, massage and ultrasound may provide temporary relief, but rarely provide long-term benefits. Exercise programs should be individualized by a spine-oriented physical therapist. Typically, the exercise program can be performed at home without special equipment. Follow-up visits with the therapist are necessary to “fine tune” the program. Returning to work in any capacity is strongly recommended.
When should I consult a doctor?
See your doctor if you have a fever, if the pain worsens, if the pain progressively moves from your back into your leg(s), or if your pain is unrelieved at rest or disturbs sleep. These are warning signs or “red flags” that require prompt, urgent medical attention.